Home » Posts tagged 'cancer care'
Tag Archives: cancer care
A Caregiver’s Medical Support Role

Photo: http://www.nlm.nih.gov
Caregivers you absolutely must be learning about the medications.
As your patient’s loved one or medical caregiver, you need to be informed about the medications that they are receiving and that you will be administering, for two critically important reasons.
1. The caregiving partner needs to monitor the side effects for the cancer patient
Assume the cancer patient is suffering from diarrhea, or nausea, and terrible headaches after a round of chemotherapy treatment. The cancer patient is in no condition to assess whether or not the situation is critical and a run to the Emergency Room / a call to your Oncologist is warranted.
But, to make this decision on the patient’s behalf, the caregiver needs to be informed of the potential side effects and their severity that are listed in the pharmacological description of the the medication. Ask questions, get help; but ultimately you are the only one who is home along face-to-face with your loved one.
So, where does the caregiver get this kind of information, you ask? The information sources that I found to be the most helpful were:
- The Internet {see the sources listed in order of informational importance and easy of understanding in Exhibit 4 of Cancer Caregiver Roles } Especially useful were the sources listed as Five Star. I would encourage caregivers to become familiar with the format and information of: WebMD, MedicineNet, and the American Cancer Society
- The Pharmacological Description of any medication provided by the pharmacy along with your prescription; these are very informative and will detail the potential side effects.
If the caregiver or patient have any questions, or cannot reach the Oncologist, a call to the Pharmacist where the prescription was filled may be helpful. Remember, you are not alone! Your Oncologist, Nurse Practitioner, or your Pharmacist are there to be of help to you. So, do not hesitate to seek help – your loved one depends on it.
The caregiver needs to be informed to be able to provide helpful information or to ask intelligent questions in meetings with the Oncologist or Oncology team. The caregiver needs to become the semi-pro, home nursing, player to be useful to the Oncologist, the team, and the patient.
Many times your patient will not be in an alert physical or mental state to follow and understand the office conversations, or to formulate questions. Your loved one/patient relies on YOU to be figure out what needs to be asked. The caregiver may surely want to make notes during meetings for reference at home later on down the road.
it is sometimes hard to remember and transfer the technical directions given in the Oncologist’s office back at home, where the passage of a few days may obscure your clarity of understanding that you seemed to experience in the office. This is when taking notes is essential.
The caregiver is in a unique position to help the Oncology team to fully understand the full holistic needs of their patient. Remember, your Oncologist may see your loved one only once or twice a month (with additional time for thinking, recording notes, and research); but you live with your patient – 24/7!
The caregiver plays a crucial role here. You must implement the day-to-day parts of the oncology treatment plan. Long time direct contact and full time, full range assistance of your loved on can greatly support and inform the Medical Team and improve your loved one’s quality of care.
And remember, NEVER be afraid to speak up or ask for help!
Frequently Asked Questions
 I wrote Cancer Caregiver Roles to help answer questions. I am here to shed light on three major roles a Caregiver must assume once their loved one/patient is diagnosed. This week’s post is a little less about Caregiving and a little more about why I do what I do. Feel free to leave me your comments or any additional questions that you may have about my work.
I wrote Cancer Caregiver Roles to help answer questions. I am here to shed light on three major roles a Caregiver must assume once their loved one/patient is diagnosed. This week’s post is a little less about Caregiving and a little more about why I do what I do. Feel free to leave me your comments or any additional questions that you may have about my work.
- Q: What inspired you to write this book?
From p. 2 Dedication: “to honor Family Caregivers—-that exhausting, noble, deepest expression of human love. And to honor my deceased wife Susan Marie.” It is my hope that her stories built into the text will “…teach and inspire them to become more loving and more proficient in their new life journey together.” When I was asked this question in another interview, I remember concluding the response like this. Truth be told, I really don’t remember any noble or altruistic motivation when I sat down to write. I only remember I HAD TO WRITE this book. Maybe it was a lifetime of teaching that subliminally drove me to share our experiences with other newly diagnosed cancer patients. Teachers are supposed to prepare their students for what is to come, and suggest ways they can succeed or survive. The key line in a Commencement Address that I gave at the University of Colorado was ” I hope we have taught you how to live, as well as how to make a living.” Maybe the Teacher experiences took over and forced the authorship of this book.
- Q: Who did you write this book for?
I had in mind the newly diagnosed cancer patient—maybe in mid-life, who has the most to lose financially. When we first went to the Cancer Center for chemo infusion in 2001 almost everyone in the room was from the older geriatric generation. I remember looking around the room during our last chemo in 2009 maybe a third of the patients were in their 30’s to 50’s. Many sat tubed up to the chemo bags, with children or todlers playing at their feet or coloring in books. Sometimes dad was there walking out in the garden with one or two of the children. Cancer diagnosis is coming to a much younger generation…and these usually have the tightest resources. If mom is going to be here for 3 – 4 hours, arrangements have to be made for children.
This book was written for CANCER patients, focusing on the definitions, treatments and diagnoses particular to the cancer journey. But it applies to ANY debilitating and progressive disease—MS, Diabetis, rheumatoid arthritis, ALS, …
It replicate and use the same diagnostic procedures, and caregiving requisites. Only the definitions and tretments are specific to cancer. And the chapters on LAUGHTER (pp 73….) and EPILOGUE on END OF LIFE are universal in their applications.
- Q: Did you find it difficult to relive some of your past experiences when writing?
Of course. There were many times I stopped typing to just read over what I had just written, and pray or cry. But my experience with the dying as a volunteer with Hospice has taught me that GRIEF is the internal black hole in your heart, stemming from the deep sense of loss. You can’t get around grief; you have to get through it. And MOURNING is the outward expression of grief. It makes you face the realities you have experienced….and appreciate the final gifts you each gave to each other. Only the expression of grief–mourning–is cathartic, and gets you through it. This book allowed me to chronicle our final gifts to each other, and as such, it was tremendously relieving.
- Q: What tips can you give us for time management?
Read pp. 68 – 72. This question sounds so academic: “Time management.” The reality of caregiving involves a deeper and swirling involvement in just holding everything together. The best metaphors I can think of for cancer are a swirling vortex sucking you into oblivion, or falling into an  unexpected quicksand where you cannot feel any bottom, and you feel yourself sinking relentlessly until the mud covers your face…..and you cannot breathe. The best tip I can give is to remain in touch with a close group of friends, or someone you can call to talk to. It becomes a planned event just to get to the grocery store for food.
unexpected quicksand where you cannot feel any bottom, and you feel yourself sinking relentlessly until the mud covers your face…..and you cannot breathe. The best tip I can give is to remain in touch with a close group of friends, or someone you can call to talk to. It becomes a planned event just to get to the grocery store for food.
I can remember being told to take breaks, or get respite care. I would think of this as a diarrhea episode would hit…and wonder when would you get time for respite care? Caregiving easily becomes 24/7 attention and surveillance. There are no breaks, because there are no breaks in life, and this is your life now shared with your partner. And my best reminder would be to join a Support Group that meets on a regular basis, so your participation can be planned. As for tips, read the list on p.69.
- Q: What do you hope readers take away from this title?
The bottom line is, cancer is extremely expensive to diagnose and treat. My wife was on a daily medication to inhibit estrogen from feeding the cancer cells; this came to $56,000 per year ($4737/per month, p.44). She had one chemotherapy regimen that was $48,000 for three months. We had treatments that totalled more than $100,000 alone; we include oncologists and physicians, diagnostic procedures, and lab work, and the total for the year came to $197,725. (p.44). It was like this for THE LAST FOUR YEARS. I found a way to cap the financial hemmorage: the “Out-of-Pocket Maximum Plan,” or stop loss plan (p.44).
THE NORMAL EVERYDAY-COUPLE NEEDS TO KNOW THIS! If they face the cancer journey without this information, they will predictable lose their savings, and possibly their home. Over 70% of all bankruptcies in America have a medical basis, and 80% of these bankruptcy victims had 80% – 20% insurance….and many go on to lose their homes as well (p.42). In the above example, if we had opted for 80% – 20% insurance, I would have had to pay 20% of $197,725. or roughly $39,545. out of our own resources. Suppose my wife had needed a stem cell transplant, or surgery to remove the large brain lesion around her brain stem; add another $150,000. Now we owe 20% of $347,725. or $69,545 out of our own pocket! The common middle class person just cannot sustain these costs. But we are talking about your loved one, your life partner, your spouse. Your impulse is to do “whatever it takes” to keep her alive. Everyday middle class couples are facing these crises on a daily basis in America.
It is the common experience of cancer couples: You get diagnosed with a terrifying disease, and it crushes you financially as well—unless you are somehow well prepared and informed.
Tumor Markers: What are they?
Tumor markers are substances that can be detected in high-than-normal amounts in the blood, urine, or body tissues of some patients with certain types of cancer. A tumor marker may be made by a tumor itself or by the body in response to the tumor.
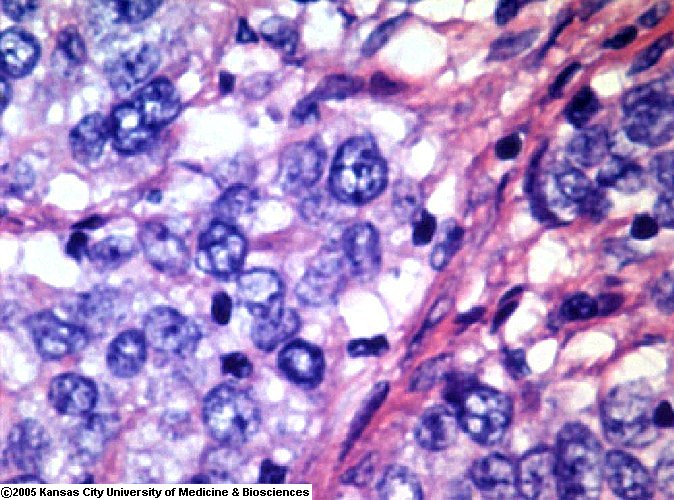
Cancer Cells. Photo via http://www.pathguy.com
Although tumor markers are typically imperfect as screening tests to detect occult (hidden) cancers, once a particular tumor has been found the marker may be used as an indicator for monitoring the success or failure of treatment. The tumor marker level may also reflect the extent or the stage of the disease, indicate how quickly the cancer is likely to progress and so help determine the prognosis.
CA 27-29: A marker that is found in the blood of most breast cancer patients. CA 27-29 levels may be used in conjunction with other procedures (such as mammograms and measurements of other tumor marker levels) to check for recurrence in women previously treated for stage II and stage III breast cancer. CA 27-29 levels can also be elevated by cancers of the colon, stomach, kidney, lung, ovary, pancreas, uterus, and liver.
CA 125: is a protein that is a so-called biomarker, which is a substance that is found in greater concentration in tumor cells that in other cells of the body. In particular, CA 125 is present in greater concentration in ovarian cancer cells that in other cells.
CEA [Carcinoembryonic Antigen] is a protein found in many types of cells but associated with tumors in the body and fetus growth. CEA is tested in blood. The main use of CEA is as a tumor marker, especially with intestinal cancer. The most common cancers that elevate CEA are in the colon and rectum. Others include:
- Pancreas
- Stomach
- Lung
- Breast
- Certain types of Thyroid cancer
CEA levels over 20 ng/ml are associated with cancer which has already metastasized (spread). A riding CEA level indicates progression or recurrence of the cancer. CEA is useful in monitoring the treatment of CEA-rich tumors; if the CEA is high before treatment, it should fall to normal [<5.0 ng/ml] after successful therapy.
It would be wise for the Caregiver to become familiar with the particular marker associated with the type of cancer diagnosed for the patient. You can then participate in following or “tracking” the effects of treatment, or conversely the growth of cancer reflected in the blood stream. These are not measures, but rather an indicator of the directions taken by the disease.
You can trace the general progression or containment of your loved one’s cancer by following these markers or indicators.
[See column number 6 of Lab Results, Exhibit 2b.]
Are you looking for some advice in your Caregiver Role? I am happy to help in anyway that I can – send me your questions via the contact form, or leave me a comment. I will get back as quickly as I can.